The Mental Health Crisis In Ghana: Insufficient Psychiatrists And The Path Forward
Table of Contents
The Stark Reality: Insufficient Psychiatrists in Ghana
Current Statistics and Data:
Ghana suffers from a drastically low ratio of psychiatrists to its population. Precise figures vary depending on the source, but estimates consistently paint a grim picture. The World Health Organization (WHO) reports a significantly lower number of psychiatrists per capita in Ghana compared to regional and international averages. This disparity is further exacerbated by an uneven distribution, with urban areas possessing a disproportionately higher concentration of mental health professionals compared to rural communities. This leaves vast swathes of the population with extremely limited access to specialized care.
- Psychiatrist-to-population ratio: Estimates suggest less than 1 psychiatrist per 100,000 people, compared to WHO recommended ratios significantly higher. (Source: [Insert credible source, e.g., Ghanaian Ministry of Health report]).
- Regional disparities: Greater Accra Region has a higher concentration of psychiatrists than the Northern, Upper East, and Upper West Regions, creating significant geographical barriers to accessing care. (Source: [Insert credible source]).
- Limited specialist availability: A shortage is also seen in other mental health professionals, such as psychologists, psychiatric nurses, and social workers, compounding the issue. (Source: [Insert credible source]).
Consequences of the Shortage:
The consequences of this severe psychiatrist shortage are profound and far-reaching. Individuals struggling with mental health issues face excessively long wait times for appointments, often exceeding months or even years. This delay in accessing appropriate treatment can lead to:
- Worsening of conditions: Untreated or delayed treatment can exacerbate existing conditions, leading to increased hospitalizations, disability, and even suicide.
- Increased suicide rates: The lack of access to timely mental healthcare is a significant contributing factor to the already concerning suicide rates in Ghana.
- Strained healthcare system: The overburdened healthcare system is further stressed by the inability to provide adequate mental health services, impacting the overall quality of care offered.
- Increased social burden: Untreated mental illness contributes to increased social burden through lost productivity, family distress, and social isolation.
Underlying Causes Contributing to the Crisis
Limited Training and Educational Opportunities:
The lack of robust training programs for psychiatrists and other mental health professionals significantly contributes to the shortage. Ghana needs to substantially increase the number of training positions and improve the quality of its training programs.
- Limited training slots: The limited number of training slots in psychiatry within Ghanaian medical schools fails to meet the current and projected future needs.
- Funding constraints: Insufficient funding for training programs hampers the ability to attract and retain qualified faculty and provide necessary resources for effective training.
- Brain drain: Many trained mental health professionals emigrate to countries offering better salaries and working conditions, exacerbating the shortage.
Stigma and Social Attitudes Towards Mental Illness:
Deep-rooted stigma and negative social attitudes surrounding mental illness represent a substantial barrier to seeking help. Cultural beliefs and traditional practices often overshadow modern medical interventions, hindering effective treatment.
- Cultural stigma: Many Ghanaians associate mental illness with witchcraft, spiritual possession, or weakness, leading to shame and reluctance to seek professional help.
- Fear of discrimination: The fear of social exclusion, discrimination, and judgment prevents many individuals from disclosing their mental health struggles.
- Preference for traditional healers: Many individuals prefer traditional healing methods over seeking help from medical professionals.
Inadequate Funding and Resource Allocation:
The insufficient allocation of government funds to mental healthcare significantly hampers the development of infrastructure, provision of equipment, and recruitment of staff.
- Low budgetary allocation: The mental health budget is disproportionately low compared to other healthcare sectors, reflecting a lack of prioritization.
- Under-resourced facilities: Many mental health facilities lack adequate resources, including essential medications, equipment, and qualified personnel.
- Limited infrastructure: A scarcity of specialized mental healthcare facilities, particularly in rural areas, further restricts access to care.
Pathways to Improve Mental Healthcare Access in Ghana
Increasing Training and Education Opportunities:
Expanding training opportunities for psychiatrists and other mental health professionals is crucial. This necessitates strategic investments in:
- Establishing more training programs: Increasing the number of training positions in medical schools and other institutions.
- Offering scholarships and incentives: Providing financial assistance and other incentives to attract individuals to mental health professions.
- Creating mentorship programs: Pairing experienced professionals with trainees to support their development and enhance their skills.
Addressing Stigma Through Public Awareness Campaigns:
Large-scale public awareness campaigns can effectively challenge the stigma surrounding mental illness and promote help-seeking behaviors. This could involve:
- Media campaigns: Utilizing television, radio, and social media to disseminate accurate information and challenge negative stereotypes.
- Community outreach programs: Organizing workshops and community events to educate people about mental health issues and encourage help-seeking.
- Educational initiatives in schools: Integrating mental health education into school curricula to promote early awareness and reduce stigma among young people.
Investing in Infrastructure and Resources:
Significant investment in mental healthcare infrastructure and resources is vital. This involves:
- Increasing the mental health budget: Allocating a substantially larger portion of the national budget to mental healthcare.
- Prioritizing infrastructure development: Constructing new facilities and upgrading existing ones to provide modern and adequate care.
- Investing in telehealth technologies: Utilizing technology to expand access to mental healthcare services in remote areas.
Integrating Mental Healthcare into Primary Care:
Integrating mental healthcare services into primary care settings can significantly increase accessibility for a broader population. This approach can:
- Reduce barriers to access: Make mental healthcare services more easily available to individuals who may not otherwise seek specialized care.
- Early identification and intervention: Enable early detection and treatment of mental health conditions, improving outcomes.
- Cost-effective approach: Potentially lead to more cost-effective mental health service delivery.
Conclusion:
The mental health crisis in Ghana, driven by a severe shortage of psychiatrists and inadequate resources, demands immediate and comprehensive action. Successfully addressing this multifaceted challenge necessitates a coordinated, multi-pronged approach. We must prioritize increasing training and educational opportunities, launching impactful public awareness campaigns to combat stigma, investing significantly in infrastructure and resources, and effectively integrating mental healthcare into primary care. By working collaboratively and committing to these critical steps, Ghana can make substantial progress towards ensuring equitable and accessible mental healthcare for all its citizens. Let's collectively strive to improve mental healthcare access in Ghana and build a future where everyone has the opportunity to receive the support they need to lead healthy and fulfilling lives.
Featured Posts
-
 Australias Opposition Promises 9 Billion Budget Improvement
May 02, 2025
Australias Opposition Promises 9 Billion Budget Improvement
May 02, 2025 -
 Dual Sense Ps 5 Controller Colors A Complete 2025 Buying Guide
May 02, 2025
Dual Sense Ps 5 Controller Colors A Complete 2025 Buying Guide
May 02, 2025 -
 6 9
May 02, 2025
6 9
May 02, 2025 -
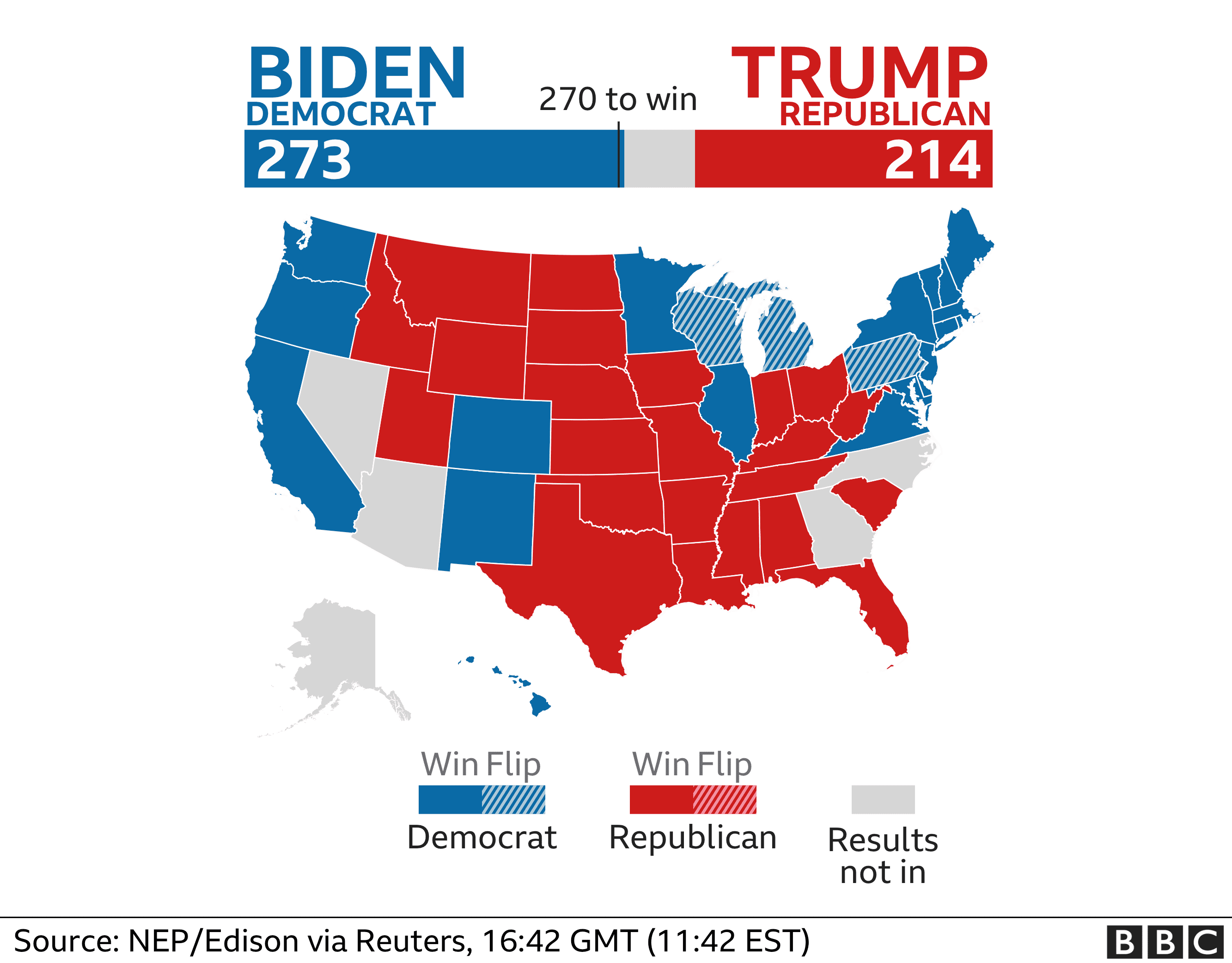 Securing Elections The Robustness Of The Poll Data System
May 02, 2025
Securing Elections The Robustness Of The Poll Data System
May 02, 2025 -
 The Missing Piece Souness On Arsenals Premier League Failure
May 02, 2025
The Missing Piece Souness On Arsenals Premier League Failure
May 02, 2025
Latest Posts
-
 Celebrity Stylist Elizabeth Stewart Designs Exclusive Capsule Collection For Lilysilk
May 10, 2025
Celebrity Stylist Elizabeth Stewart Designs Exclusive Capsule Collection For Lilysilk
May 10, 2025 -
 Elizabeth Stewart X Lilysilk Spring 2024 Collaboration Unveiled
May 10, 2025
Elizabeth Stewart X Lilysilk Spring 2024 Collaboration Unveiled
May 10, 2025 -
 Elizabeth Stewart And Lilysilk Partner For A Stunning Spring Collection
May 10, 2025
Elizabeth Stewart And Lilysilk Partner For A Stunning Spring Collection
May 10, 2025 -
 Elizabeth Hurleys Bikini Fashion A Maldives Vacation Diary
May 10, 2025
Elizabeth Hurleys Bikini Fashion A Maldives Vacation Diary
May 10, 2025 -
 Maldives Vacation Elizabeth Hurleys Bikini Looks
May 10, 2025
Maldives Vacation Elizabeth Hurleys Bikini Looks
May 10, 2025
